April 21, 2020
|
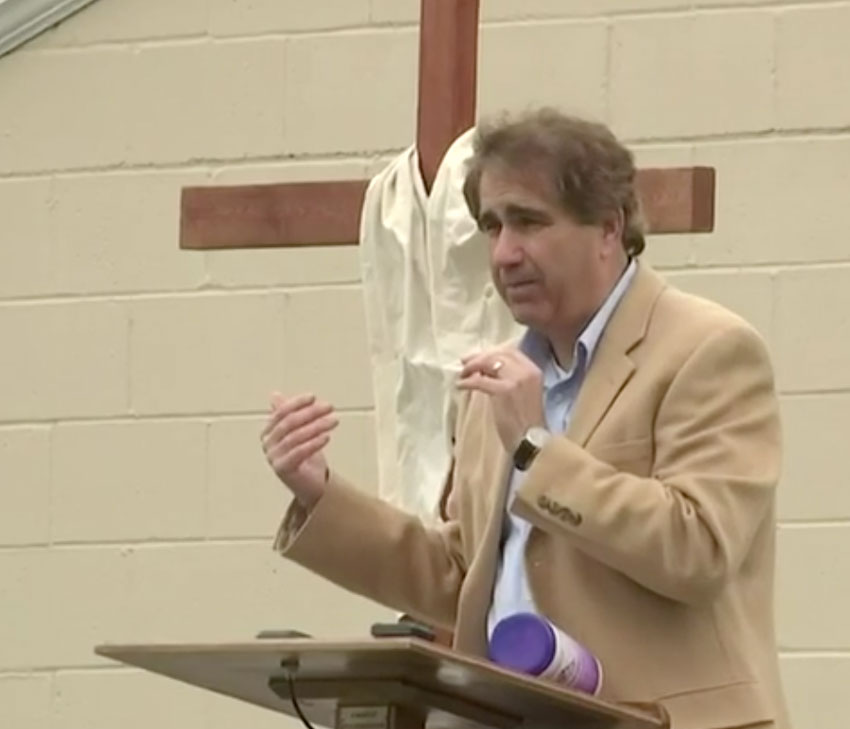
 UB Global missionaries Dr. Richard and Cathy Toupin (right) are currently working at the Samaritan’s Purse field hospital in Central Park, New York. They spent the first few months of the year at Mattru Hospital in Sierra Leone, but were forced to return to Indiana early because of the pandemic.
UB Global missionaries Dr. Richard and Cathy Toupin (right) are currently working at the Samaritan’s Purse field hospital in Central Park, New York. They spent the first few months of the year at Mattru Hospital in Sierra Leone, but were forced to return to Indiana early because of the pandemic.
Before the Toupins left for New York, UB Global spoke with them in a public videochat. The Toupins talked about how Mattru Hospital was preparing for the coronavirus.
Sierra Leone was among the last countries in the world to have Covid-19 cases, reporting its first case on March 31. As of April 21, there are 43 confirmed cases, and no deaths. Says Richard, “They are doing significant social distancing. The government has been very aggressive and proactive in closing the borders, preventing flights from going in and out, and restricting movement within the country.”
Around the end of February, they recognized that Covid-19 was spreading globally and would eventually come to Sierra Leone. So the hospital leadership began making preparations. The senior medical staff now consists of one physician being seconded by the Nigerian government, and three community health officials (CHOs).
Richard: “One thing the hospital has lacked for many years is a fence around the hospital. Community members take many different paths through the hospital grounds. So the first thing was to put a temporary fence around the hospital. About the time we began this plan, we received a $10,000 grant from the Southwestern Medical Foundation. Part of that money was used to build this fence. It has been completed, so now the hospital has borders, and people are not crossing through the hospital as much as they were.”
In 2014 during the Ebola epidemic, the hospital built a triage building. That has been rehabilitated. They also created an isolation unit for Covid-19 patients, using a ward built initially for tuberculosis patients. In addition, the government set up testing capabilities at the hospital to test for Covid-19. Says Richard, “There has been a very good relationship between the hospital and the district health medical team.”
Cathy: “When we had our meetings, the head lab guy said they would be able to test without taking the actual samples back to their lab, so that everything else wouldn’t get contaminated.”
Richard addressed the lack of PPE (Personal Protective Equipment). “During the Ebola years, the whole world was focused on the three countries of West Africa affected by Ebola, so all of these supplies came into Sierra Leone, Liberia, and Guinea. That’s not the case now. While we were there, we were scrambling to determine where we would get PPE. It turns out there was a really good supply of masks left over from the Ebola days. They had thousands of masks, but some were damaged during their time in storage. The local government hospital on Bonthe island, downriver from Mattru, had lots of gowns but they didn’t have masks. So we exchanged that kind of PPE. Unfortunately, there’s a real need for gloves, and hopefully the government will be able to step in to supply that PPE when the time arises.
“As far as we know, there is one ventilator in the country. To put that in perspective, there are 10.6 million people in Sierra Leone, and just one ventilator at a private hospital. It is quite awful to think about the consequences of what will happen if this becomes widespread in Sierra Leone. About 85% of people do well with this illness, but 15-20% don’t do well and need to be hospitalized. Of those, a high number need to be on high-flow oxygen, and a smaller percentage, 3-4%, end up on ventilators.”
Richard said portable oxygen cylinders are uncommon in the developing world. At Mattru, they have large storage containers, and oxygen is piped into rooms. “So the only option in rural Sierra Leone is to use an oxygen concentrator. They require electricity, and over time they wear out. Part of the recent grant money is earmarked for oxygen concentrators, but the problem is getting them into the country, especially now that there is very little shipping coming into Sierra Leone.”
Cathy: “We have only one oxygen concentrator that is working right now. We used to have three, and we bought a new one while we were there, but it lasted a week and then broke. So at this point there is only one oxygen concentrator. We’re trying to get two more, but the whole world is needing them, and we don’t know if we’ll be able to get any more. We do have somebody coming to look at the old ones to see if they can be prepared, but they definitely need something to give oxygen to these patients.”
A solar grid was installed at Mattru Hospital in 2017. Some technical issues remain, but it has been a huge blessing to the hospital.
Richard: “Having 24-hour electricity is something we in the West take for granted. If the power goes out for an hour or two, we kind of freak out. In Sierra Leone, a significant portion of the country doesn’t have 24-hour electricity, and the same is true for the town of Mattru Jong. Having electricity 24 hours a day has been revolutionary for the hospital. It has allowed the lab to work 24 hours a day, and has provided lights into the maternity ward, power for the operating room, and power for oxygen concentrators when they are functioning. So it has revolutionized the care.”
 Nadine Louise Speas, 88, passed away April 25, 2020, in Grand Ledge, Mich. She is survived by her husband, George, to whom she was married in 1955. George was ordained as a United Brethren minister in 1987, and they served in the pastorate for many years in Michigan, including 30 years at Kilpatrick UB church (Woodland, Mich.). A private burial will take place in the Woodland Memorial Park Cemetery, with a public celebration of Nadine’s life to be held at a later date.
Nadine Louise Speas, 88, passed away April 25, 2020, in Grand Ledge, Mich. She is survived by her husband, George, to whom she was married in 1955. George was ordained as a United Brethren minister in 1987, and they served in the pastorate for many years in Michigan, including 30 years at Kilpatrick UB church (Woodland, Mich.). A private burial will take place in the Woodland Memorial Park Cemetery, with a public celebration of Nadine’s life to be held at a later date.
 UB Global missionaries Dr. Richard and Cathy Toupin (right) are currently working at the Samaritan’s Purse field hospital in Central Park, New York. They spent the first few months of the year at Mattru Hospital in Sierra Leone, but were forced to return to Indiana early because of the pandemic.
UB Global missionaries Dr. Richard and Cathy Toupin (right) are currently working at the Samaritan’s Purse field hospital in Central Park, New York. They spent the first few months of the year at Mattru Hospital in Sierra Leone, but were forced to return to Indiana early because of the pandemic.
 On Good Friday, UB Global missionaries Dr. Richard and Cathy Toupin (right) left for New York City to work with Samaritan’s Purse in treating COVID-19 patients. Last September, they attended an SP conference in Florida, during which they signed up to be part of a Disaster Assistance Response Team. After Palm Sunday, they received a call: you’re needed in New York. They have committed to work there for three weeks, until May 1, and could opt to extend it another two weeks.
On Good Friday, UB Global missionaries Dr. Richard and Cathy Toupin (right) left for New York City to work with Samaritan’s Purse in treating COVID-19 patients. Last September, they attended an SP conference in Florida, during which they signed up to be part of a Disaster Assistance Response Team. After Palm Sunday, they received a call: you’re needed in New York. They have committed to work there for three weeks, until May 1, and could opt to extend it another two weeks. Erik and Iris Rojas (right) lead the one United Brethren church in Costa Rica. Pastor Rojas sent a message on April 9. He said they’ve had about 500 cases of Covid-19 since the first case was confirmed on March 6 (an American tourist from New York), and there have been two deaths. But thanks to tough restrictions from the government, they appear to have the curve under control. He then sent the following information about his church in San Jose.
Erik and Iris Rojas (right) lead the one United Brethren church in Costa Rica. Pastor Rojas sent a message on April 9. He said they’ve had about 500 cases of Covid-19 since the first case was confirmed on March 6 (an American tourist from New York), and there have been two deaths. But thanks to tough restrictions from the government, they appear to have the curve under control. He then sent the following information about his church in San Jose.